EHR-Agnostic Revenue Cycle Integration
We work seamlessly with major EHR and Practice Management platforms to ensure smooth data exchange, reduced friction, and real-time accessibility — all without disrupting your workflow. Our integration supports efficiency at every step of the revenue cycle.
Prevent Revenue Leakage at the Source
Capture charges with precision to prevent revenue loss
and reduce Days in A/R. Boost denial overturn rates
and accelerate your overall revenue
cycle performance.
Smarter, Actionable RCM Insights
Monitor clean claim rates, denial patterns, and collections
with real-time insights that reveal hidden issues.Make faster, data-
backed decisions to optimize your revenue
cycle performance.
HIPAA-Compliant, Scalable Infrastructure
Stay audit-ready and secure with future-proof systems that adapt to regulatory
changes and long-term growth.
Our infrastructure ensures HIPAA compliance through
encryption, role-based access, and automated audit trails.
EHR-Agnostic Medical Billing System
We integrate with all major EHRs and PMs, ensuring real-time data exchange, minimal workflow disruption, and full compatibility across your revenue cycle.
Prevent Revenue Loss and Delays
Capture every charge accurately, reduce Days in A/R, and improve denial resolution rates to protect and accelerate your cash flow performance.
Smarter Analytics for Faster Decisions
collections with real-time insights to drive faster, data-backed financial decisions.
HIPAA
Compliant Scalable Cloud Platform
systems built to scale with regulatory changes and your
growing practice needs.
End-to-End RCM Solutions
Faster Cash Flow Predictability
We reduce Days in A/R with timely claim submission and follow-ups. Underpayments are recovered and write-offs minimized—ensuring steady and predictable revenue.
Accurate Coding, Better Revenue
Our certified coders specialize across medical disciplines to deliver clean, compliant coding that accelerates reimbursements and reduces denials.
Scalable RCM for Any Practice
RCM Automation
That Works
Whether you are a solo provider or a growing group, our solutions scale seamlessly with your needs—without sacrificing speed or accuracy.
Specialties We Serve
Why Partner with RCmediX Health ?
Unleash Your Practice’s Full Financial Potential
Automated Efficiency & Financial Control
Streamline operations, boost profitability, gain end-to-end financial oversight.
Actionable Insights & Superior Analytics
Real-time data for strategic RCM optimization and informed decisions.
Expert Coding & Specialty Precision
Seamless Integration & Scalable Solutions
Connects with any EHR/PMS, flexible to grow with your practice.
Proactive Compliance & Dedicated Support
Built-in regulatory adherence and personalized support for peace of mind.
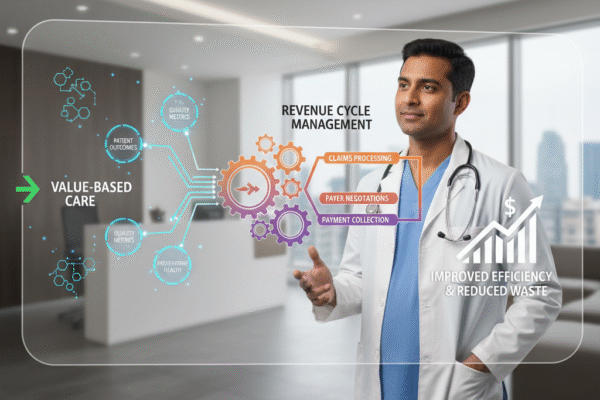
Optimized for Value-Based Care
Drive better outcomes and maximize reimbursements in new healthcare models.
Our Core RCM Services Include

Credentialing: Streamlining Your Path to Network Participation & Revenue Provider credentialing is the essential first step for any healthcare professional or organization to bill for services and participate in insurance networks. At RCMediX Health , our expert credentialing services remove the complexity and administrative burden of medical credentialing and payer enrollment. We meticulously manage every detail to ensure your providers are accurately and efficiently credentialed—safeguarding your revenue cycle and accelerating reimbursement from day one. Why Expert Provider Credentialing is Crucial for Your Practice Accelerated Revenue: Expedited credentialing means faster approval for network participation, allowing you to bill and receive reimbursement sooner, directly impacting your financial health. Prevent Claims Denials: Incorrect or lapsed provider enrolment is a leading cause of claims denials. Our precision minimizes these costly rejections, improving your RCM efficiency. Reduced Administrative Burden: Free your administrative staff from the intricate, paper-heavy credentialing process, allowing them to focus on patient care and in-house operations. Guaranteed Compliance: We ensure all applications and re-applications adhere to the latest regulatory requirements and payer guidelines, protecting your practice from compliance risks. Our Comprehensive Provider Credentialing Services 1. Initial Provider Credentialing & Payer Enrolment New Provider Setup: We handle the entire medical credentialing process for new providers joining your practice or existing providers seeking network participation for the first time. Application Management:From gathering necessary documentation to preparing and submitting applications to all relevant commercial payers, Medicare, and Medicaid. CAQH ProView Management: We efficiently set up and maintain your CAQH ProView profile, a critical hub for streamlined provider enrolment. Licensure & Certification Verification:Meticulous verification of all professional licenses, certifications, and educational backgrounds to meet payer requirements. Accelerated Onboarding: Our streamlined process significantly reduces the time it takes for your new providers to become billable, directly impacting revenue cycle management. 2. Provider Re-credentialing & Maintenance Timely Renewals: We proactively manage re-credentialing deadlines, ensuring all necessary documentation is updated and submitted well in advance to prevent any lapse in network participation. Continuous Monitoring:Ongoing monitoring of provider licenses, DEA registrations, and malpractice insurance to ensure continuous compliance. Proactive Updates: We handle all necessary updates to CAQH ProView and payer profiles as provider information changes. Prevent Service Interruptions: Our diligent re-credentialing prevents any disruption in your ability to bill for services, safeguarding consistent reimbursement. Compliance Assurance: Ensures your practice remains fully compliant with all evolving payer and regulatory requirements for provider enrolment. 3. Network Participation & Contract Management Support Strategic Enrolment: We assist in identifying and applying for network participation with payers most relevant to your patient demographic and service lines. Contracting Facilitation: While we don’t negotiate contracts, we facilitate the exchange of necessary documentation between your practice and payers for new agreements. Fee Schedule Verification: We help verify that your practice is correctly loaded with agreed-upon fee schedules post-enrolment to ensure accurate reimbursement. Ongoing Relationship Management: We maintain communication with payer credentialing departments to expedite processes and resolve any issues. Maximizing Access: Our services ensure your providers are linked to the right networks, maximizing patient access and your potential healthcare revenue. 4. NPI & PECOS Management NPI Application & Updates: We manage the application for and any necessary updates to your National Provider Identifier (NPI) for both individual (Type 1) and organizational (Type 2) entities. PECOS Enrolment & : We handle enrollment and ongoing maintenance within the Medicare Provider Enrolment, Chain, and Ownership System (PECOS), crucial for Medicare reimbursement. EHR Integration Support: Ensuring NPI and PECOS information is correctly linked within your electronic health records (EHR) and medical billing systems. Compliance Backbone: Accurate NPI and PECOS registration is a fundamental requirement for claims submission and compliance across all payers. Streamlined Billing: Proper NPI and PECOS management prevents common claims denials related to provider identification, ensuring smoother payment recovery.

Payment Recovery: Payment Recovery Optimization Recover every dollar you’ve earned through structured A/R follow-up and patient collections. Aged A/R Segmentation: We categorize your outstanding receivables by payer, aging bucket, and balance, targeting the most recoverable claims first. Targeted Follow-Up Workflows: Specialized teams manage payer-specific follow-ups using denial codes, escalation protocols, and status tracking to resolve claims faster. Underpayment Analysis: We compare allowed vs. paid amounts against contracts, flag discrepancies, and recover underpaid claims through reprocessing and appeals. Patient Balance Recovery: Our team helps communicate transparently with patients, enabling collections through respectful engagement and flexible payment plans. Timely Appeal Submissions:Structured appeals with supporting documentation are submitted within deadlines to overturn denied claims and maximize collections. Strategic Denial Management: Reduce preventable denials and build a smarter, more compliant RCM process. Denial Root-Cause Analysis: We track and report the top denial reasons (eligibility, prior auth, coding errors), and implement permanent fixes. Payer-Specific Denial Patterns: Insights into frequent denial behaviors by payers help refine billing rules and renegotiate contracts where necessary. Preemptive Edits & Flags: Front-end edits and custom rules in the clearinghouse prevent known denial triggers before claims are submitted. Appeals Strategy & Tracking: Each denial is classified and routed to the appropriate appeal pathway with ongoing status monitoring and escalation when needed. Prevention Through Education: We provide denial education to front-desk, billing, and coding teams, creating upstream improvements across the revenue cycle. Advanced Reporting: Make smarter decisions with real-time, specialty-focused analytics and KPIs. RCM Performance Dashboards: Visual dashboards track key metrics such as denial rate, DSO, net collections, and clean claim rate—all updated in real time. Custom Reports by Specialty: Whether you’re a hospital, ASC, or specialty clinic, reports are customized to track what matters most for your operations. Drill-Down Data Views: Zoom into claim-level, payer-level, or provider-level performance to identify revenue leaks or operational inefficiencies. Alerts & Exception Reporting: Receive alerts for missed billing timelines, underpayments, and trends that need attention, enabling faster response and correction. Client-Facing Transparency: All reporting is available to clients on-demand, ensuring full visibility and trust in your revenue cycle operations. Predictive Revenue Forecasting: Plan for growth, mitigate risks, and allocate resources more strategically. Revenue Trend Projections: We use historical and current data to project future revenue, giving your leadership better financial foresight. A/R Cash Flow Modeling: Forecast expected recoveries across A/R aging buckets to support stable cash flow planning. Denial Volume Forecasting: Anticipate spikes in denial trends by season, payer, or specialty to strengthen front-end mitigation strategies. Business Intelligence for Expansion: Use insights to evaluate potential service line additions, location expansion, or provider performance optimization. Scenario-Based Planning: Plan for “what-if” scenarios like payer changes, policy updates, or staffing shifts with smart forecasting tools. Operational Performance & Compliance Analytics: Ensure your processes, people, and documentation meet the highest standards. Staff Productivity Tracking: Measure billers’, coders’, and follow-up agents’ output by volume, speed, and success rate to optimize performance. Workflow Bottleneck Analysis: Identify operational slowdowns (e.g., in prior auth or charge entry) and redesign workflows for better throughput. Audit-Ready Documentation: Maintain clean audit trails with consistent tracking of payer communications, appeal actions, and claim history. KPI Benchmarking: Compare your performance against industry and specialty benchmarks to identify improvement areas and competitive advantage. Regulatory Compliance Checks: Ensure ongoing compliance with CMS, HIPAA, and payer policies through documentation audits and automated alerts.

Authorization & Benefits Verification :Securing Your Revenue Before the Claim Starts In the complex world of healthcare revenue cycle management (RCM), success begins at the front-end. At RCMediX Health , our integrated Authorization & Benefits Verification services proactively address coverage issues and financial risks before the point of care—drastically reducing denials, improving collections, and elevating the patient experience. Comprehensive Benefits Verification Real-Time Eligibility Checks: We instantly verify patient eligibility with commercial, Medicare, and Medicaid payers—confirming active coverage, effective dates, and policy status. Detailed Payer Coverage Insights: Our team analyzes plan-specific benefits including co-pays, coinsurance, deductibles, visit limits, and out-of-pocket maxes—ensuring no detail is overlooked. Service-Specific Verification: We identify whether the scheduled procedure or service is covered, what requirements apply, and uncover any restrictions that may delay billing. Automated Workflows for Speed & Accuracy: Our AI-enhanced tools process high volumes of verifications efficiently, reducing manual work while improving accuracy and throughput. Upfront Patient Cost Tra to reduce ansparency: By providing a full breakdown of patient responsibility, practices can improve front-desk collections, reduce billing disputes, and build patient trust. Prior Authorization Management Proactive Authorization Identification: We determine exactly which services require prior approval—before the visit happens—to avoid costly payment denials. Full Authorization Handling: Our experts manage the entire lifecycle of each prior authorization—from payer submission and documentation to status tracking and appeals. Compliance with Complex Rules: With our rigorous workflows, all authorizations are submitted on time and monitored actively to ensure there are no care delays or revenue loss. Regulatory Compliance & Audit Protection: We secure required authorizations for every case, helping you meet payer rules and protecting you from compliance-related penalties. Financial Counseling & Patient Education Accurate Cost Estimates: Based on verified benefits, we help staff deliver clear financial estimates to patients—preventing surprises and enabling informed decision-making. Payment Plan Setup: We support your front-desk team with resources to discuss financial responsibility and offer payment options when needed. Improved Data Integrity: Transparent communication about coverage and costs improves the patient experience, reduces payment friction, and increases loyalty. Integrated RCM Workflows Seamless Integration with Billing & Coding: Our professional fee codingOur verification processes are fully embedded into your revenue cycle, ensuring claim accuracy and front-end data consistency. AI-Driven Optimization: Intelligent automation identifies potential benefit issues early, flags inconsistencies, and continuously improves intake processes. Reduced Rejections & Improved Cash Flow: Front-end accuracy leads to cleaner claims, fewer rejections, and faster reimbursements—keeping your revenue cycle predictable and strong.

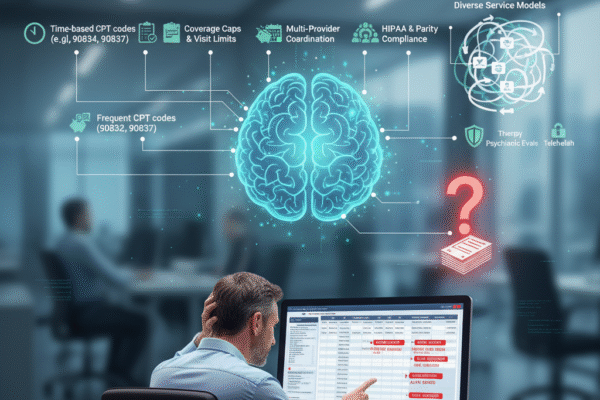
Medical Coding Services: Precision for Your Revenue Cycle At RCMediX Health , we understand that precise medical coding is the foundation of a healthy revenue cycle. Our certified coders expertly translate complex clinical documentation into accurate ICD-10-CM, CPT, and HCPCS codes—ensuring compliance, reducing denials, and securing the reimbursement you deserve. Partner with RCmediX Health to transform clinical data into lasting financial strength. Our Specialized Medical Coding Services Include 1. Comprehensive Medical Coding Services End-to-End Accuracy: We provide meticulous medical coding services across all specialties, ensuring every patient encounter is accurately represented.. Certified Expertise: Our team comprises highly qualified, certified medical coders (CPC, CCS, etc.) who stay abreast of the latest coding guidelines and regulatory changes. Faster Reimbursement:Accurate coding translates directly into clean claims, significantly accelerating your payment recovery and cash flow within the revenue cycle. Reduced Denial Rates: By ensuring precision at the coding stage, we proactively prevent common denial management issues related to incorrect coding. Streamlined Workflows:Outsource your coding to us to reduce administrative burden on your staff, allowing them to focus on patient care. 2. Expert Facility Coding Services Hospital & ASC Specialization:We provide specialized facility coding services for hospitals (inpatient and outpatient), ambulatory surgery centers (ASCs), and other institutional settings. DRG & APC Optimization: Our coders are experts in assigning accurate Diagnosis-Related Groups (DRGs) and Ambulatory Payment Classifications (APCs) to optimize reimbursement. Compliance with Complex Rules: We navigate the intricate rules of facility coding, including Charge Master integration and payer-specific guidelines. Operational Efficiency:Streamlining facility coding processes ensures a faster journey from patient discharge to claim submission. Audit Readiness: Our meticulous approach ensures your facility coding records are robust and ready for any payer or regulatory audit. 3. Specialized Risk Adjustment Coding Services Accurate HCC Capture:We specialize in risk adjustment coding services, meticulously identifying and coding Hierarchical Condition Categories (HCCs) for accurate patient risk profiles. Optimal Payment Calculation: Correct HCC coding is crucial for health plans and providers participating in value-based care models, directly impacting capitated payments and financial performance. Improved Data Integrity: Our risk adjustment coding ensures that clinical documentation fully supports the patient’s severity of illness and chronic conditions. Audit Support: We help ensure your risk adjustment coding practices meet CMS and payer audit requirements, minimizing compliance risks. Strategic Revenue Growth: By accurately reflecting patient complexity, our services help you achieve fair and appropriate reimbursement in risk-adjusted models. 4. Professional Fee Coding Services Physician & Provider Focus: Our professional fee coding services are tailored for individual physicians, group practices, and various specialties (e.g., surgical, E/M, anesthesia). E/M, Surgical & Ancillary Coding:Expertise across all service types, ensuring accurate application of Evaluation and Management (E/M) codes, surgical procedures, and ancillary services. Payer-Specific Nuances: We understand the subtle differences in professional fee coding requirements across diverse payers, minimizing rejections. Maximized Physician Rest claims compared to imbursement: Accurate coding directly impacts the reimbursement for physician services, safeguarding your professional income. Reduced Administrative Burden: Free up your clinical staff from coding complexities, allowing them to concentrate on patient care. 5. Documentation Integrity Audits Proactive Risk Mitigation: Our documentation integrity audits identify potential compliance risks and coding errors before they impact your revenue cycle. Enhanced Accuracy: We meticulously review medical records to ensure that documentation fully supports the codes assigned, strengthening your claims. Compliance Assurance: Audits verify adherence to official coding guidelines (ICD-10-CM, CPT, HCPCS) and regulatory requirements, minimising audit liabilities. Identify Revenue Opportunities: Beyond compliance, our audits can uncover missed coding opportunities, helping to optimize your reimbursement. Continuous Improvement: Provides actionable feedback and training opportunities for your clinical and coding teams, fostering ongoing excellence in documentation and revenue cycle management.

Medical Billing Excellence: Your Pathway to Accelerated Collections Our precision-driven, technology-enhanced medical billing services ensure every claim is accurate, every payment is captured promptly, and your practice’s financial performance is consistently optimized. While you focus on delivering exceptional patient care, we’ll take care of your cash flow—efficiently and expertly. Key Components of Our Medical Billing Service 1. Precision Patient Registration & Demographic Management Foundation of Accuracy: We begin by meticulously capturing and verifying all patient demographics and insurance details. Error Prevention: Our rigorous process eliminates common data entry mistakes that lead to costly claim rejections down the line. Seamless Integration: Patient information flows seamlessly into the billing process, ensuring consistency from the start. Compliance Assured: We adhere to strict data privacy and security protocols (e.g., HIPAA) for all patient information. Reduced Administrative Burden: Your staff is freed from tedious manual data checks, allowing them to focus on patient interaction.. 2. Comprehensive Charge Capture & Entry Maximized Revenue Capture: Every service rendered is accurately documented and translated into billable charges. Eliminate Missed Charges: Our systematic approach ensures no procedure or consultation goes unbilled, protecting your earned revenue. Coder-Biller Alignment: We facilitate clear communication between clinical documentation and billing codes for optimal accuracy. Timely Processing: Charges are entered swiftly to accelerate the claim submission timeline. Financial Integrity: This crucial step maintains the financial integrity of your services and operations. 3. Proactive Claims Scrubbing & Quality Assurance First-Pass Resolution: Our advanced scrubbing technology automatically identifies and corrects potential errors before claims are submitted. Denial Prevention: We meticulously check for coding inconsistencies, missing information, and payer-specific rules, drastically reducing initial denials. Increased Acceptance Rates: Clean claims submitted right the first time lead to higher acceptance rates and faster reimbursements. Compliance Adherence: Ensures all claims meet the latest regulatory and payer requirements, minimizing audit risks. Efficiency Gains: Automating the error-checking process saves valuable time and resources for your team. 4. Accelerated Electronic Claims Submission Swift Transmission: We ensure the rapid and secure electronic submission of all claims to commercial, Medicare, and Medicaid payers. Optimized Payer Connections: Leveraging direct connections, your claims reach the right destination without delay. Reduced Payment Lag: Faster submission directly translates to quicker processing and accelerated cash flow for your practice. Error-Free Delivery: Electronic submission minimizes manual errors and lost claims compared to paper processes. Real-Time Tracking: Provides the foundation for monitoring claim status and ensuring timely receipt by payers. 5. Meticulous Payment Posting & Reconciliation Accurate Financial Records: All insurance and patient payments, adjustments, and denials are precisely posted to the correct accounts. Daily Reconciliation: We meticulously balance posted payments with bank deposits, ensuring full financial transparency and preventing discrepancies. Faster Dispute Resolution: Accurate posting allows for quick identification of underpayments or errors, facilitating rapid appeals. Enhanced Audit Readiness: Comprehensive and precise records simplify internal audits and external reviews. Clear Financial Overview: Provides a real-time, accurate snapshot of your practice’s current financial standing. 6. Strategic Payer Communication & Follow-Up Proactive Claims Management: We don’t wait for denials; we actively track claim statuses and engage with payers to resolve issues. Expedited Resolutions: Our dedicated team effectively communicates with insurance companies to address delays, discrepancies, and denials. Reduced A/R Days: Persistent and informed follow-up drastically cuts down the time claims remain unpaid in accounts receivable. Expert Navigation: We understand complex payer policies and processes, ensuring your claims are handled correctly. Revenue Protection: Safeguarding your revenue by aggressively pursuing and recovering outstanding reimbursements.
Proven by Results
The RCMediX Health Advantage
We don’t just promise performance — we deliver it. Every number tells a story of reduced costs, improved collections, and enhanced satisfaction. Our track record speaks for itself.
Costs Reduced
Maximize margins with streamlined RCM operations.
Reduction in Days in AR
Accelerate cash flow with faster collections.Clean Claim Rate
Minimize rejections and denials from the start.Client Satisfaction
Trusted by practices for our reliability and service quality.
EHR Systems Supported
Seamless integration with all major platforms.Medical Specialties Served
Tailored expertise for diverse care disciplines.
Who We Serve
Empowering Healthcare Providers To Simplify RCM, Accelerate Revenue, And Stay Compliant.
RCmediX Health supports a wide range of healthcare organizations with tailored revenue cycle solutions.

Physician
Groups

Hospitals
From community hospitals to large systems, we ensure clean claims, efficient workflows, and scalable support.

Behavioral Health Providers

Skilled Nursing Facilities (SNFs)
Specialty Providers
Unlock Your Revenue Potential
Discover how RCMediX Health can streamline your revenue cycle, reduce denials, and boost profitability—no matter your specialty or size.
Testimonial
Our Reputation Is Built on Precision and Care
Partnering with RCmediX Health completely transformed our revenue cycle. Our cash flow improved dramatically, and their proactive denial management cut rejections to a minimum. We finally have full financial visibility, and our team can focus on patient care—not paperwork. RCmediXHealth is a game-changer for any digestive health practice.

Dr. Sanjay
Digestive Health PracticeFor a psychiatric practice, clarity in billing is paramount. RCmediX Health brings exactly that. They've streamlined our complex claims, leading to fewer headaches and more predictable revenue. This partnership genuinely simplifies our financial operations, allowing our focus to remain on healing.

Dr. Debbie
Psychiatric SpecialistEHR-Agnostic Compatibility
We Work With Your EHR — No Matter the Platform
RCmediX Health is fully EHR-agnostic, meaning we seamlessly integrate with over 30+ leading EHR and Practice Management Systems. Whether you’re using Epic, Cerner, Kareo, NextGen, eClinicalWorks, or any other platform — we meet you where you are.
Our team ensures smooth data exchange, minimal disruption, and maximum efficiency, so your RCM processes remain unified and stress-free.










Get Started
Let’s Talk About Your Revenue Goals
We’re ready to help you simplify your revenue cycle, reduce administrative burden, and boost your bottom line. Reach out today.