Behaviour Health
Transforming Behavioural Health Billing and Coding Efficiency
Revenue Cycle Management (RCM) is revolutionizing behavioural health billing and coding — reducing denials, streamlining workflows, and boosting financial performance for mental health and TMS practices.
1.Introduction
Behavioural health providers play a crucial role in addressing mental health and substance use challenges — yet they often operate within one of the most complex billing environments in healthcare.
Unlike general medical billing, behavioural health revenue cycle management (RCM) involves varied payer policies, session-based CPT codes, and strict compliance standards. These complexities often result in claim denials, delayed payments, and administrative burdens.
To overcome these challenges, many behavioural health practices are now adopting AI-driven RCM solutions that combine automation, analytics, and intelligent workflows to improve billing accuracy, accelerate reimbursements, and sustain financial growth.
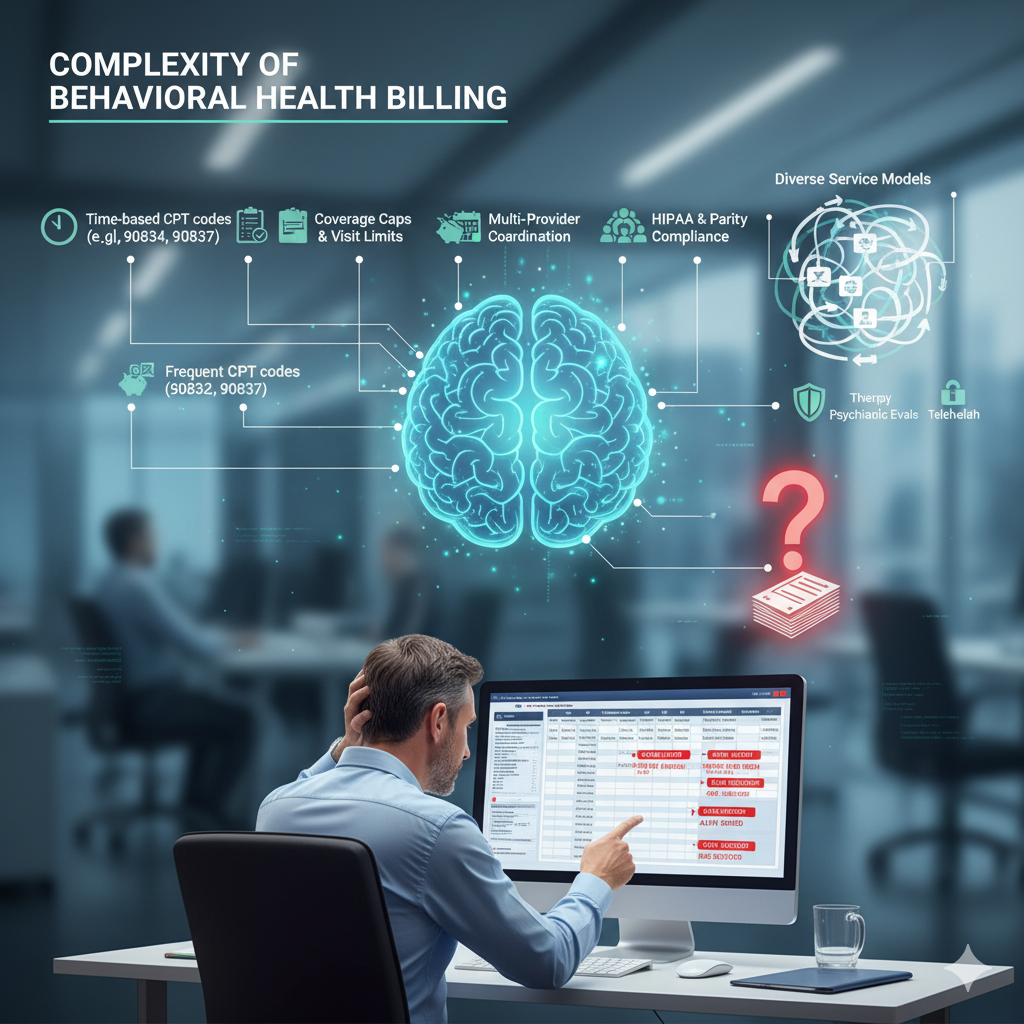
2.Understanding the Complexity of Behavioural Health Billing
- Behavioural health billing differs from other medical specialities due to its diverse service models, ranging from therapy sessions and psychiatric evaluations to telehealth visits. Key challenges include:
-
• Time-based CPT codes requiring precise documentation (e.g., 90832, 90834, 90837)
• Frequent pre-authorizations for therapy or substance use programs
• Coverage caps and visit limits imposed by payers
• Multi-provider coordination (psychiatrists, therapists, counselors)
• Strict compliance under HIPAA and parity regulations - These factors make expertise and automation essential to maintaining accuracy and compliance.
3. Top Behavioural Health Billing & Coding Challenges
-
1 .Top Behavioural Health Billing & Coding Challenges
Every payer follows unique reimbursement guidelines. Even identical CPT codes may differ in coverage, documentation, or session limits, leading to confusion, denials, or payment delays.
-
2. Time-Based Coding and Multi-Session Documentation
Behavioural health billing relies on accurate session-time documentation. Misalignment between the recorded duration and billed CPT code often results in claim denials or audits.
-
3. Prior Authorization and Service Limitations
Many behavioural health services require prior authorization. Expired or missing approvals remain a leading cause of revenue leakage and claim rejection.
-
4. Compliance and Policy Changes
Frequent CMS and payer updates — especially around telehealth and parity laws — require continuous monitoring. Missing updates can lead to noncompliance and penalties.
-
5. Lack of EHR-Billing System Integration
When EHRs and billing systems are disconnected, data duplication and manual entry errors become inevitable, reducing efficiency and increasing denials.
-
6. High Denial and Rejection Rates
Behavioural health practices face above-average denial rates due to missing information, incorrect codes, or insufficient documentation — requiring costly rework.
-
7. Workforce and Training Limitations
Non-specialized billing teams may lack the expertise for time-based codes, modifiers, and payer-specific nuances — impacting collections and compliance.
Smart Solutions: How to Overcome Behavioural Health Billing Challenges
-
1. Adopt AI-Powered RCM Platforms
AI-enabled RCM solutions can detect claim errors, predict denials, and automate manual workflows.
Core AI capabilities include:
• Automated eligibility and benefits verification
• Predictive denial analytics
• Smart claim scrubbing and coding validation
• Automated A/R and denial worklists
• NLP-based clinical note analysis for coding accuracy
This enhances first-pass claim acceptance rates and significantly reduces administrative workload.
-
2. Strengthen Documentation and Coding Precision
Ensure all session notes capture:
• Duration and modality
• Therapeutic methods
• Patient progress
• Medical necessity justification
Certified behavioural health coders and periodic audits are key to maintaining compliance and reimbursement accuracy.
-
3. Automate Authorization and Coverage Tracking
AI-driven authorization tracking tools alert teams before approvals expire — minimizing missed renewals and denials.
-
4. Integrate EHR and RCM Systems
Seamless integration ensures real-time data flow between clinical documentation and billing, improving transparency, accuracy, and revenue forecasting.
-
5. Partner with Behavioural Health RCM Specialists
Outsourcing to RCM experts provides access to certified coders and billing professionals who specialize in behavioral health payer requirements.
They manage:
• Eligibility and authorizations
• Coding and charge entry
• Denial management
• Payment posting and reconciliation
• Analytics and reporting
This approach reduces overhead while improving consistency and cash flow.
-
6. Leverage Data Analytics for Revenue Optimisation
Monitoring KPIs like denial rates, days in A/R, and collection percentages enables continuous performance improvement.
AI-based analytics help identify underpayments, track payer trends, and optimize revenue operations.
-
7. Enhance Patient Billing Experience
Clear statements, digital payment options, and AI-based patient communication tools improve transparency and reduce unpaid balances — a major win for behavioural health practices with recurring sessions.
The Future: AI-Powered Behavioural Health RCM
-
AI is redefining how behavioural health organizations manage their revenue cycles.
Emerging AI applications include:· Predictive Denial Management: Prevent rejections before they occur.
· RPA (Robotic Process Automation): Streamline repetitive billing tasks.
· AI-Assisted Coding: Suggest accurate CPT and ICD-10 codes based on clinical documentation.
· Real-Time Dashboards: Track key financial metrics instantly. - Together, these tools can reduce administrative effort by up to 40%, improve cash flow by 20%, and ensure long-term financial resilience.
Conclusion
Behavioural health practices face growing financial pressures — from payer complexity to documentation demands.
By adopting AI-driven RCM solutions, providers can automate routine billing tasks, reduce denials, and gain real-time insight into their revenue cycle.
This technology-driven approach enables practices to focus on what truly matters: delivering quality care while achieving financial stability and growth.
Get Started
Unlock the Full Revenue Potential of Your Practice
RCMediX Health helps transform coding from a risk area into a strategic advantage. Contact us today for a consultation and learn how accurate coding can drive measurable financial improvement.