
Accurate Medical Coding
Unlock Hidden Revenue and Minimize Denials
Medical coding errors cost the U.S. healthcare system approximately $36 billion annually in lost revenue, denied claims, and compliance penalties, according to JAMIA. A 2022 Crowe RCA benchmark study revealed that 11% of all claims were denied, equating to over 110,000 unpaid claims for a typical health system. These figures underscore the critical importance of medical coding accuracy for healthcare organisations of all sizes.
For private multi-specialty practices, physician groups, and Ambulatory Surgery Centers (ASCs), especially those handling over 1,000 visits monthly, coding precision is a major determinant of financial health. RCMediX Health brings nearly 20 years of U.S. RCM experience to support practices in preventing revenue leakage and reducing denials.
The Hidden Cost of Coding Errors
Coding mistakes are more than operational issues—they directly impact profitability and compliance.
- 1. Upcoding: Billing for a more complex or expensive service than what was actually provided is not just incorrect—it’s fraudulent. This invites audits, fines, and legal risk.
- 2. Undercoding: Commonly due to insufficient documentation or coder caution, undercoding results in lost revenue. Services performed must be accurately represented to ensure fair reimbursement.
- 3. Unbundling Errors: Billing individual components of a procedure separately instead of using a bundled code can trigger immediate denials. Understanding bundling rules is essential.
- 4. Modifier Misuse: Improper use or omission of modifiers, such as 22, 25, or 59, can lead to rejections or compliance scrutiny. Each modifier must align with clinical documentation.
- 5. Medical Necessity & Incomplete Documentation: Claims must reflect both the service and medical need. Missing information in clinical notes can result in denials, audits, and regulatory violations.
- 6. Duplicate Billing & POS Errors: Submitting the same service multiple times or using incorrect Place of Service codes damages credibility and delays payment.
- 7. ICD-10 Specificity & NCCI Edits: Using vague diagnoses or ignoring NCCI guidelines leads to avoidable claim rejections and audit risks.
The Strategic Role of Certified Coders
Certified coders act as revenue protectors by:
- Understanding CPT, ICD-10-CM, and HCPCS Level II guidelines
- Navigating payer-specific coding nuances
- Interpreting complex documentation accurately
- Ensuring coding compliance to avoid penalties
A certified coding team is critical for specialties with high procedural volume, such as dermatology, cardiology, neurology, or orthopedics.
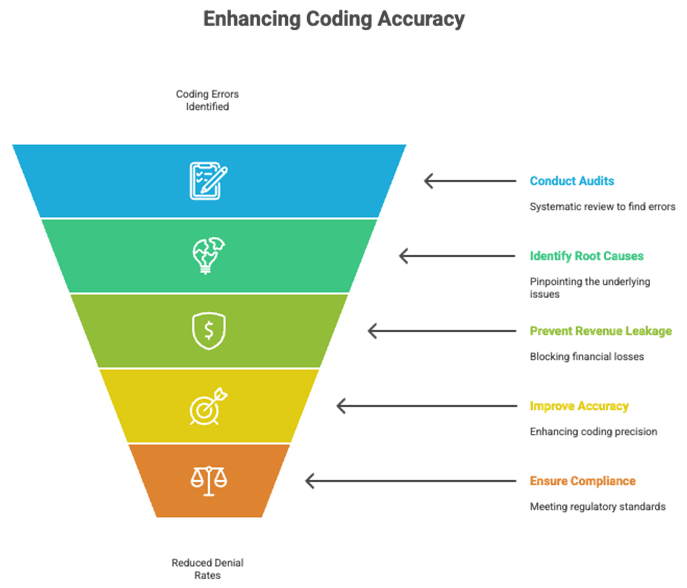
Strengthening Accuracy Through Audits and Training
Routine Coding Audits
- Identify recurring errors and root causes
- Prevent revenue leakage before it impacts cash flow
- Improve coding accuracy and ensure regulatory compliance
Ongoing Training & Provider Education
- Update teams on changing coding guidelines and payer requirements
- Strengthen documentation habits to support accurate billing
- Boost team performance and reduce coder burnout
For large groups, quarterly audits and monthly education sessions can drastically reduce denial rates.
The Power of Technology in Coding Optimization
Technology enhances coder performance and protects revenue by:
- AI-Powered Code Suggestions: Accelerates coding with suggested codes based on documentation.
- Claim Scrubbing Tools: Flags errors and missing data before submission.
- Integrated Code Libraries: Keeps CPT, ICD-10, and HCPCS codes updated.
- Advanced Reporting Dashboards: Track denial trends and claim success rates.
- EHR Integration: Seamlessly connects with systems like Athenahealth, Kareo, eCW, AdvancedMD, NextGen, and DrChrono.
For urgent care centers and high-volume specialties, this leads to faster reimbursements and a reduced administrative burden.
Why Choose RCmediX Health for Medical Coding Services?
With a focus on accuracy, compliance, and revenue optimization, RCMediX Health delivers:
- Reduced Denials: Submit clean claims with compliant coding and documentation.
- Higher Reimbursements: Prevent undercoding and capture full revenue potential.
- Stronger Compliance: Stay aligned with CMS and payer guidelines.
- Improved Cash Flow: Get paid faster with fewer rejections.
RCmediX Health supports professional and facility coding across a wide range of specialties. Our certified team, combined with advanced RCM technology, ensures coding excellence tailored to your operational needs.
FAQs: Medical Coding Simplified
A: It can lead to claim denials, lost revenue, compliance audits, and even legal penalties.
A: Through certified coders, technology-driven audits, real-time claim edits, and proactive documentation support.
A: Inaccurate or incomplete codes trigger denials, impacting both revenue and administrative efficiency.
A: Tools like claim scrubbers, integrated code updates, and documentation-to-code validation improve accuracy and speed.
A: Multi-specialty practices, ASCs, and physician groups handling high patient volumes and complex procedures.
Get Started
Unlock the Full Revenue Potential of Your Practice
RCMediX Health helps transform coding from a risk area into a strategic advantage. Contact us today for a consultation and learn how accurate coding can drive measurable financial improvement.
Get Started
Unlock the Full Revenue Potential of Your Practice
RCMediX Health helps transform coding from a risk area into a strategic advantage. Contact us today for a consultation and learn how accurate coding can drive measurable financial improvement.
