Strategic Revenue Cycle Management
In-House vs Outsourced or Hybrid Models for Optimal Healthcare Financial Health
In the increasingly complex and competitive landscape of healthcare, efficient Revenue Cycle Management (RCM) and meticulous medical billing are not merely administrative functions; they are the strategic pillars of financial solvency and sustainable growth. As regulatory frameworks continually evolve and economic pressures mount, healthcare providers face a critical operational decision: to manage their medical billing in-house, to partner with a specialized outsourced medical billing provider, or to strategically adopt a hybrid medical billing model.
There is no singular, universally "best" approach. The optimal choice for your healthcare entity – whether a multi-specialty hospital, a specialized clinic, or an individual practitioner – hinges on a nuanced evaluation of your unique operational needs, existing resources, and long-term healthcare revenue optimization goals. This comprehensive guide delves into the distinct advantages and inherent challenges of each model, empowering you to make an informed decision that secures your practice's financial vitality.
In-House Medical Billing
For decades, the traditional approach involved managing medical billing entirely within the confines of the practice. This model necessitates the establishment and maintenance of a dedicated internal team responsible for the entire RCM process, from patient demographic capture and insurance eligibility verification to claims submission, denial management, and final payment posting.
Operational Definition
- In-House Billing Operations: This signifies direct employment of billing personnel, proprietary investment in billing software and IT infrastructure, and comprehensive internal accountability for all RCM and medical coding activities.
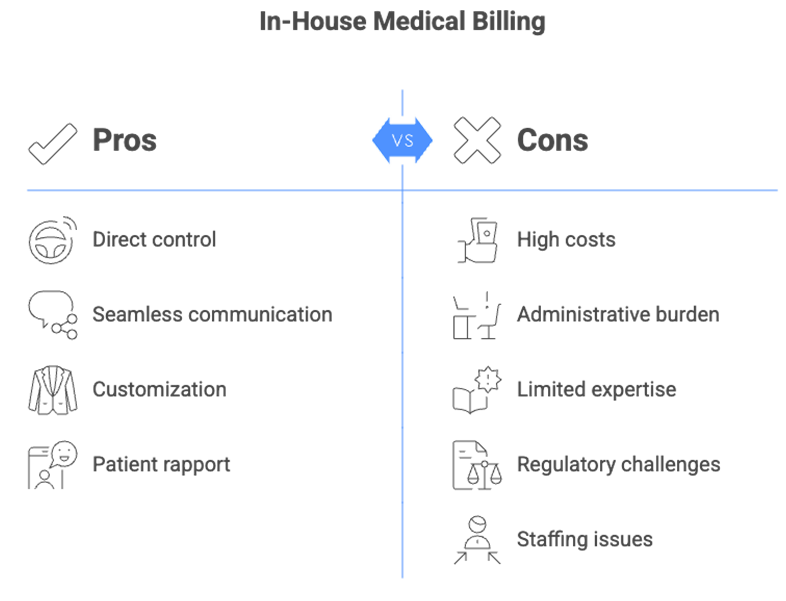
Strategic Advantages
- Direct Control and Granular Oversight: This model offers unparalleled authority over every facet of medical billing operations. Practices retain the flexibility for immediate process adjustments and maintain direct accountability, fostering a sense of complete command over sensitive financial data.
- Seamless Local Communication and Patient Rapport: Proximity facilitates rapid, highly personalized communication between billing specialists, front-desk staff, and clinical teams. This ensures swift resolution of patient inquiries regarding bills, enhancing the overall patient experience and fostering stronger patient relationships.
- Tailored Customization and Adaptability: Internal processes can be precisely customized to align with your practice's unique clinical workflows, specific patient demographics, and intricate local payer contracts. This high degree of flexibility supports bespoke operational adjustments.
- Data Proximity and Enhanced Security Perception: For organizations with stringent internal data governance policies or specific concerns regarding data residency, maintaining billing data managed entirely on-site (even if utilizing cloud-based software) can offer a perceived additional layer of control and data security.
Inherent Challenges
- Significant Overhead and Unforeseen Costs: This often represents the most substantial financial deterrent. Beyond direct salaries and benefits, practices incur substantial costs for continuous staff training (especially for specialized certifications), licensing for advanced billing software, hardware maintenance, and the allocation of dedicated office space and utilities.
- Talent Acquisition, Retention, and Expertise Gaps: Recruiting and retaining skilled, experienced medical coders and billers in a competitive talent market can be arduous. High staff turnover rates, potential for burnout, and managing absences (vacations, sick leave) can severely disrupt cash flow and overall RCM efficiency. Furthermore, internal teams may struggle to maintain specialized expertise in the face of constantly evolving medical coding updates, complex denial management strategies, or nuanced payer rules across diverse geographies.
- Burdensome Compliance Management: The complete onus of staying abreast of and adhering to constantly evolving regulatory frameworks – including global standards like HIPAA (where applicable for cross-border services) and national mandates – falls squarely on the internal team, requiring substantial dedicated resources and expertise.
- Scalability Limitations: Significant fluctuations in patient volume can lead to either an overburdened billing team struggling to keep pace, or underutilized staff, resulting in operational inefficiencies. Achieving efficient scalability without incurring considerable hiring or downsizing costs becomes a significant challenge.
- Diversion from Core Clinical Focus: The substantial administrative burdens associated with managing a complex RCM process can divert invaluable physician and clinical staff time and attention away from core patient care responsibilities and strategic initiatives aimed at practice management and clinical excellence.
Outsourced Medical Billing
Outsourced medical billing entails forging a strategic partnership with a specialized third-party firm that assumes comprehensive responsibility for your RCM functions. These entities are typically industry experts, equipped with state-of-the-art technology, highly trained and certified personnel, and a profound understanding of billing complexities across diverse healthcare systems.
Core Proposition
- Outsourcing Medical Billing: This involves contracting with an external provider to efficiently manage all or specific components of your medical billing and RCM processes, leveraging their specialized infrastructure, deep expertise, and advanced technological capabilities.
Compelling Benefits for Healthcare Providers
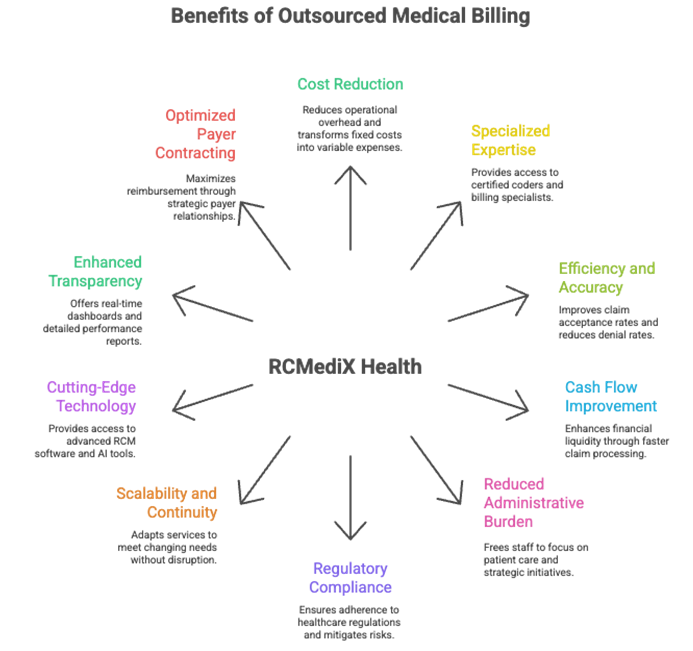
- Significant Cost Reduction and Enhanced Financial Efficiency: This is frequently the most immediate and impactful advantage. Outsourced medical billing drastically reduces your operational overhead by eliminating direct costs associated with salaries, employee benefits, continuous training, office space, and expensive proprietary software licenses. This transforms unpredictable fixed costs into a more manageable, predictable variable expense, directly enhancing your healthcare financial management and overall profitability.
- Unparalleled Access to Specialized Expertise: Reputable outsourcing companies employ highly qualified, certified medical coders, seasoned billers, and dedicated denial management specialists. They possess a profound and current understanding of intricate coding guidelines (ICD-10, CPT, HCPCS), diverse payer-specific rules, and continually updated national and international regulations. This specialized knowledge directly translates to significantly fewer claim errors, maximized legitimate reimbursements, and accelerated Accounts Receivable (A/R) cycles.
- Guaranteed Improvement in Efficiency and Accuracy: Specialized RCM outsourcing firms implement highly optimized workflows, stringent quality assurance protocols, and cutting-edge technology. This consistently leads to a substantially higher clean claim rate (claims accepted on first submission), expedited payment cycles, and dramatically lower denial rates. Their focused expertise minimizes human error and ensures claims are processed and reimbursed with superior accuracy.
- Accelerated Cash Flow and Enhanced Revenue Capture: Beyond just cost savings, outsourcing directly improves your financial liquidity. By proactively mitigating claim denials, accelerating claim processing, and implementing robust follow-up strategies for outstanding balances, it ensures a more consistent and robust cash flow for your practice. Expert RCM providers actively work to identify underbilling issues and missed revenue opportunities, and optimize net collection rates, thereby maximizing your overall revenue capture.
- Substantial Reduction in Administrative Burden: One of the most invaluable advantages is the operational freedom it provides. By offloading complex, time-consuming, and often frustrating medical billing tasks, your in-house administrative and clinical staff are liberated to fully concentrate on delivering high-quality patient care, enhancing the patient experience, and driving strategic practice growth initiatives. This elevates overall productivity and staff satisfaction.
- Proactive Regulatory Compliance and Risk Mitigation: Staying abreast of ever-changing healthcare regulations – including stringent global standards like HIPAA (for international patient data) and critical national mandates – is a monumental, full-time undertaking. Reputable outsourcing partners proactively monitor and adapt to these changes, ensuring your medical billing practices remain fully compliant with all legal and industry standards, significantly mitigating audit risks and potential penalties.
- Superior Scalability and Robust Business Continuity: Whether your patient volume experiences seasonal surges or your practice embarks on rapid expansion, outsourcing partners can effortlessly scale their services up or down to meet your evolving needs without the burden of costly hiring or downsizing cycles. Furthermore, they provide uninterrupted service, minimizing disruptions due to in-house staff turnover, vacations, or unforeseen absences, thereby ensuring a consistent and reliable revenue stream.
- Immediate Access to Cutting-Edge Technology: Gain instant access to advanced RCM software, RCM automation tools (like Robotic Process Automation - RPA), and sophisticated Artificial Intelligence (AI) and Machine Learning (ML) capabilities for predictive analytics, automated claim scrubbing, and robust reporting. This allows your practice to leverage the latest technological advancements to streamline processes, improve accuracy, and gain invaluable insights, all without requiring substantial upfront capital investment.
- Enhanced Transparency and Actionable Reporting: Leading medical billing outsourcing firms provide comprehensive, real-time dashboards and detailed reports on your RCM performance. This offers unparalleled visibility into key performance indicators (KPIs) such as clean claim rates, denial rates, Days in A/R, and net collection rates, empowering you with precise, data-driven insights to inform strategic decision-making and continuous improvement.
- Optimized Payer Contracting and Credentialing Support: Many specialized outsourced RCM providers offer expertise in payer contracting and credentialing services, ensuring your practice is optimally set up with insurance networks for maximized reimbursement and reduced administrative hurdles.
- Reduced Training & HR Overheads: Eliminate the need for continuous training programs for billing staff, as the outsourcing partner ensures their team is always up-to-date with the latest coding and billing regulations. This also significantly reduces the HR burden of recruitment, onboarding, and managing a specialized billing department.
Key Considerations
- Addressing Perceived Loss of Control: While daily operational control is outsourced, a transparent and high-performing partner provides robust reporting and maintains open communication channels to ensure comprehensive oversight.
- Ensuring Seamless Communication and Workflow Integration: Establishing clear communication protocols and defined channels is crucial to bridge the gap between your practice and the outsourced team.
- Rigorous Data Security and Compliance Due Diligence: Thorough due diligence is paramount to ensure the outsourcing partner adheres to stringent data security measures and is fully compliant with all relevant regulations, including HIPAA (for global operations) and national data privacy acts.
- EHR/PM System Integration Needs: Ensuring seamless technical integration between the outsourced provider’s RCM platforms and your existing Electronic Health Record (EHR) or Practice Management (PM) system is critical for efficient data flow.
- Strategic Partner Selection: Choosing a reliable, experienced, and culturally aligned outsourcing partner with a proven track record is vital for long-term success.
The Hybrid RCM Model
Increasingly, forward-thinking healthcare practices recognize that a “one-size-fits-all” approach may not be the optimal solution. The hybrid RCM model is emerging as a highly flexible and strategic alternative, enabling practices to selectively outsource specific RCM functions while meticulously retaining others in-house. This approach intelligently leverages the distinct strengths of both full in-house and full outsourcing models.
A. Definitional Overview
- The Best of Both Worlds: A hybrid RCM model represents a strategic collaboration where certain RCM processes are managed internally – typically those requiring direct patient interaction or close oversight – while more specialized, high-volume, or resource-intensive tasks are entrusted to an external RCM expert.
B. Strategic Advantages of a Hybrid Approach
- Optimized Control and Specialized Expertise Integration: This model allows practices to retain direct control over critical, patient-centric functions (e.g., front-desk collections, patient inquiries) while simultaneously gaining access to specialized, outsourced expertise for complex medical coding, denial management, or A/R follow-up.
- Enhanced Patient Financial Experience: By keeping patient-facing financial discussions and collections in-house, your practice can ensure a personalized, empathetic approach that perfectly aligns with your specific patient care philosophy and local community expectations.
- Achieving Balanced Cost-Effectiveness and Efficiency: This model empowers you to strategically outsource only those functions where external partners offer significant cost savings, superior efficiency, or access to advanced RCM technology, thus optimizing your overall RCM expenditure and improving net collection rates.
- Superior Scalability and Proactive Risk Mitigation: This model provides the inherent flexibility to scale specific medical billing functions up or down based on patient volume without the direct burden of expanding or contracting an entire in-house team. Distributing RCM responsibilities across both internal and external teams can also significantly diversify operational and compliance risks.
C. Common Hybrid Implementations
- In-House Front-End, Outsourced Back-End: Your administrative staff handles patient registration, eligibility verification, and co-pay collections at the point of service. The outsourced partner then assumes responsibility for complex medical coding, electronic claims submission, proactive denial management, extensive Accounts Receivable (A/R) follow-up, and accurate payment posting.
- Outsourcing Specialized or Complex Functions: Your in-house team competently manages routine medical billing, while the external partner manages challenging denial appeals, workers' compensation claims, intricate surgical medical coding, or credentialing services.
- Technology-Augmented Hybrid: Your practice invests in and utilizes advanced RCM software with automation features for initial charge capture and claim scrubbing. The outsourced partner then provides expert oversight, handles exceptions flagged by the software, conducts deep data analytics, and manages manual interventions for highly complex or problematic cases.
D. Key Success Factors for a Hybrid Model
- Meticulous Planning and Clearly Defined Roles: Success hinges on meticulously defining responsibilities and workflows for both in-house and outsourced teams to prevent duplication of effort or critical operational gaps.
- Robust Communication and Seamless Collaboration: Establishing transparent and frequent communication channels, including regular performance reviews and structured issue resolution processes, is paramount for a cohesive RCM operation.
- Seamless Technological Integration: Ensuring that your Electronic Health Record (EHR) or Practice Management (PM) systems integrate smoothly and securely with the outsourced partner's RCM platform is crucial for efficient data exchange and streamlined workflows.
Making the Optimal Choice for Your Practice: A Strategic Framework
Deciding on the optimal RCM strategy for your healthcare practice requires a thorough, objective self-assessment and a forward-looking perspective on your financial future.
A. Critical Self-Assessment Questions
- Current RCM Performance and Identified Pain Points: What are your existing clean claim rates, denial rates, Days in A/R, and cost-to-collect? Where are your most significant bottlenecks, points of revenue leakage, or areas of persistent staff frustration within your current medical billing process?
- Practice Size, Specialty, and Growth Projections: Is your practice experiencing rapid expansion? Does your medical specialty involve particularly complex medical coding or unique payer requirements that demand specialized expertise?
- Budgetary Allocations and Financial Goals: Conduct a comprehensive cost-benefit analysis of each RCM model, meticulously factoring in all direct and indirect expenses, as well as the potential for enhanced revenue capture and improved cash flow.
- Technology Infrastructure and Capabilities: Do you possess modern medical billing software and robust IT support capable of meeting your evolving RCM needs, or is a significant capital investment and upgrade necessary?
- Internal Staff Expertise and Capacity: Does your current team possess the necessary certifications, up-to-date training, and sufficient bandwidth to effectively handle the increasing complexities and volume of RCM functions?
B. Steps Towards an Informed Decision
- Conduct a Comprehensive Needs Assessment: Objectively identify your RCM strengths, inherent weaknesses, current opportunities for improvement, and potential threats to your revenue cycle.
- Thorough Research and Vetting of Potential Partners: Prioritize experienced RCM companies with a proven track record, strong client references, clearly defined Service Level Agreements (SLAs), and robust compliance measures.
- Consider a Phased Implementation Strategy: For a hybrid approach, or even a full transition to outsourcing, consider starting with a pilot program for specific functions or a gradual handover of responsibilities to ensure a seamless and risk-mitigated transition.
Conclusion
Optimizing Your Revenue Cycle for a Sustainable Future
In the fiercely competitive healthcare landscape, an impeccably optimized revenue cycle is no longer a mere operational advantage; it is an absolute imperative for financial sustainability and exponential growth. Whether your strategic choice leads you to fortify your in-house medical billing team, embrace the comprehensive benefits of full outsourced medical billing, or strategically combine both with a sophisticated hybrid RCM model, the overarching objective remains constant: to fundamentally enhance your financial health, profoundly streamline operational efficiencies, and ultimately, empower your dedicated medical professionals to focus wholeheartedly on delivering exceptional, patient-centric care.
At RCMediX Health Health, we deeply understand these intricate decisions and the unique demands of the healthcare sector. We offer flexible, tailor-made RCM solutions designed to integrate seamlessly with your practice, ensuring your revenue cycle is robust, highly efficient, and comprehensively future-proof. Partner with us to navigate the complexities of medical billing and achieve lasting financial success.
Get Started
Unlock the Full Revenue Potential of Your Practice
RCMediX Health helps transform coding from a risk area into a strategic advantage. Contact us today for a consultation and learn how accurate coding can drive measurable financial improvement.

